The 12th February 2019 was a momentous day in my calendar. I should probably acknowledge my younger brother turned 21 that day too but sorry kid my day was momentous too (I think I am more likely to remember the day than you too!).
After 17 months on a temporary contract I interviewed for the same role I had. Although relatively confident with all the funding problems there was some anxiety around it. Thankfully, like the first set of interviews a decision was made same day to offer me the contract on a permanent basis. The process happened quite near the end of the temporary contract due to funding. The monies which paid for me (as well as a large number of the team) had been short term rolling with last minute decisions. So it had taken a while to find an alternative source as everyone else was on permanent contracts and thus could be redeployed. During the interviews (as there was another applicant) an email was received stating that all teams had had their monies made permanent. Which was the second bit of amazing news for us all. There had been months of putting in the bid for the money follow by 20 months of having to prove it was value for money and being spent properly. For it to then be renewed just a few months at a time. Prior to it being made substantive this had taken up vast amounts of my time.
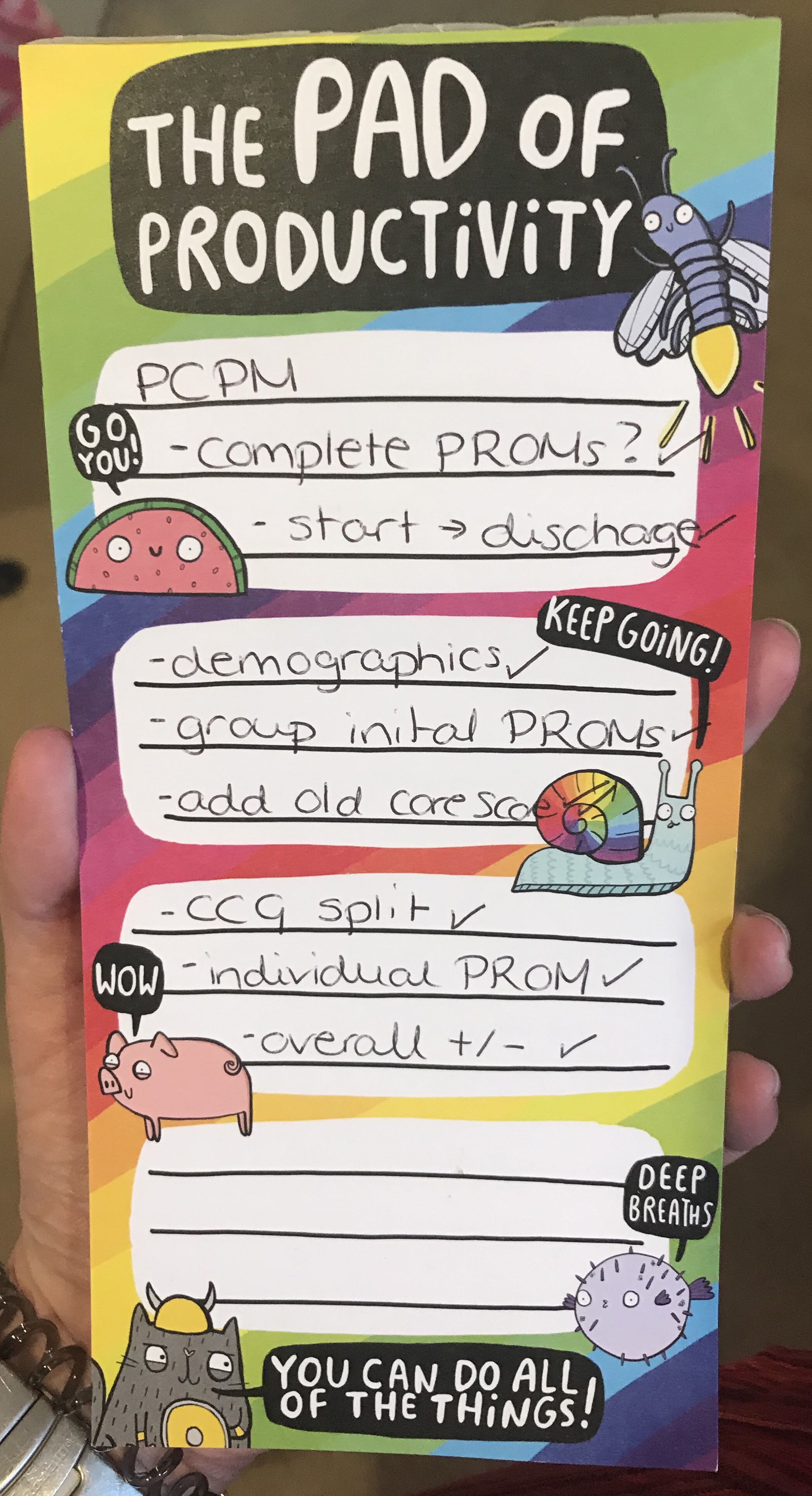
While still reeling from all this excitement we had one more notification come through which was being listed as a finalist for the BMJ awards for the PCPM (Primary Care Psychological Medicine) Project. This had already been previously listed for an HSJ award too. It is safe to say we finished the day just a little bit giddy.
So now that the monies were made permanent and that had taken up a lot of my time. What happened next? We could finally start being proactive. We could look at more interesting things than fighting fires when chaos happened. Chaos happens still, there is no doubt about that but slightly less than before.
I built my internal monitoring reports for my teams. This allows us to look at things monthly to try and see if changes are beginning to happen before they become overly problematic. It was also a good “bonding” opportunity. I sat down with the clinicians and learnt more about what concerned them. What changes had they noticed which was having an impact on them (for better or worse) but also what could change that would impact on them. So each teams is slightly different. I wanted the clinicians to feel heard, when working in such a busy high paced environment you don’t need much change from the status quo for disaster to strike. This also highlighted some problems with service equity. They had gone under the radar not due to malice or lack of care but everyone was so busy keeping the department floating no one could see past
PCPM also progressed a lot. I had been on the project a while already however this was the year progress was made. Shortly after the permanent contract is when the nomination was put in for AphA awards. This project really helped with my analytical skills. Not only did it prove to have some strong analytical challenges due to the time series of the patient cohort (everyone with a different start and end date), different lengths of time in service, the cohort had both engaged and disengaged patient, data was pulled from multiple sources and formats (including some weird date formats I hope to never see again in my life). The next aspect was considering the clinical side of these patients. When looking at service usage for this cohort of patients (Who are commonly describe as either medically unexplained symptoms, psychosomatic symptoms, persistent physical symptoms) you have to consider what can be influenced and what cannot. Pregnancy for example. Although the hope for after treatment at PCPM people would have lower anxiety and lower service usage, however pregnancy will always increase service usage even in traditionally “healthy” expectant mothers. So would skew the results. Same consideration was given to patients who had a car accident or cancer diagnosis. However we had to consider what clinically would be included or excluded.
The other new and exciting endeavor has been the training/talking/education. This all started with Chris B being asked if he knew any ladies who used R (and he quickly recommended Zoe and I). From that one talk I remembered how much I enjoyed such things. So then gave a talk at NHS-R and started planning other bits. Will hopefully be soon talking at a local APHA branch (that will likely be situated just a few paces from my office for utmost convenience, selling point for others is that it is near the tram too), will discuss my award at the APHA conference in Birmingham come September. I have been in talks with a local public health consultant about doing training at the university level for medical schools to improve medics understanding earlier. I am also running some CPD sessions in my trust for consultants.
Still on going is the planning for the HSR-UK conference. Our panel, which talks about using and linking healthcare data. Our assorted team gives a diverse approach to the data. With my focus as always being about the clinicians and inputting the data. How building those relationships are key to getting any meaningful analysis being done. I am practicing what I preach still. Jo (@Peet_Joanna) is a ward manager for the acute trust after jumping ship (not evasively!) from on of the Liaison Teams. We have remained in contact and share data and information to try and bridge the gap between mental health and acute trust. She is passionate about how improving mental health knowledge on acute wards has major benefits for patients. So we are presenting together (my data, her clinical knowledge/intervention) a poster in June.
Our research paper was submitted to a major journal and revisions requested. So I remain hopeful for that as it was not an automatic rejection. That will be my name on that paper officially and the start of hopefully many citations against my name.
A lot has also changed. Not all positive. I have faced many health challenges and they have knocked onto each other and impacted work. Far more than I wish it had. There have been a lot of changes in staffing, with some good people coming and good people going on. Becoming a cyborg was a highlight as it changed everything. It improved my life in some ways endlessly but has caused a significant number of problems too. I spent a lot of time off sick with it. A lot of time on the sofa (which is very good coding time for passion projects). It gave me a lot of time to ask other NHS staff about data. A habit of mine any hospital admission.
Looking forward to the next year. I am excited for the posters and sessions being run to improve healthcare data from both sides. I have met very few totally resistant people when it came to learning. A lot is meeting people half way and understanding the challenges. Often why is the more important question than how. I want to keep improving what is happening for Liaison in Nottinghamshire and how it affects the surrounding areas of healthcare. I have more R coding to build and develop including a current focus on PROMS. Health wise I am not after cured I am not deluded, but some stability would be a nice change!